Understanding PBMs
Understanding PBMs
satya - 1/9/2022, 12:10:59 PM
Understanding Pharmacies and PBMs
Understanding Pharmacies and PBMs
satya - 1/9/2022, 12:11:05 PM
Understanding Pharmacies and PBMs
satya - 1/9/2022, 12:13:40 PM
From Pharmacists Association of NY: pssny
satya - 1/9/2022, 12:14:11 PM
Taken from the article below: PBM Basics
satya - 1/9/2022, 12:16:31 PM
From American Health Policy.org, A PDF
satya - 1/9/2022, 12:18:15 PM
Health Premiums, Deductibles, earnings, inflation
Show images for: Health Premiums, Deductibles, earnings, inflation
satya - 1/9/2022, 12:23:12 PM
As of 2019 (from 2009), looking up some graphs there
1. inflation 20%
2. wages 26%
3. Premiums 54%
4. deductibles 162%
satya - 1/9/2022, 12:30:00 PM
IT of PBMs
1. Manage a retail network of pharmacies
2. Mail order capabilities
3. Drug quantity purchasing discounts
4. clinical analysis
5. eligibility tracking and determination
6. Claims adjudication
7. Payments to pharmacies
satya - 1/9/2022, 12:43:16 PM
Accumulators and PBMs Architecture
satya - 1/9/2022, 12:43:38 PM
An example of a PBM platform: Nirvana
satya - 1/9/2022, 1:14:32 PM
How do pharmacies check prior authorization?
How do pharmacies check prior authorization?
satya - 1/10/2022, 7:56:39 AM
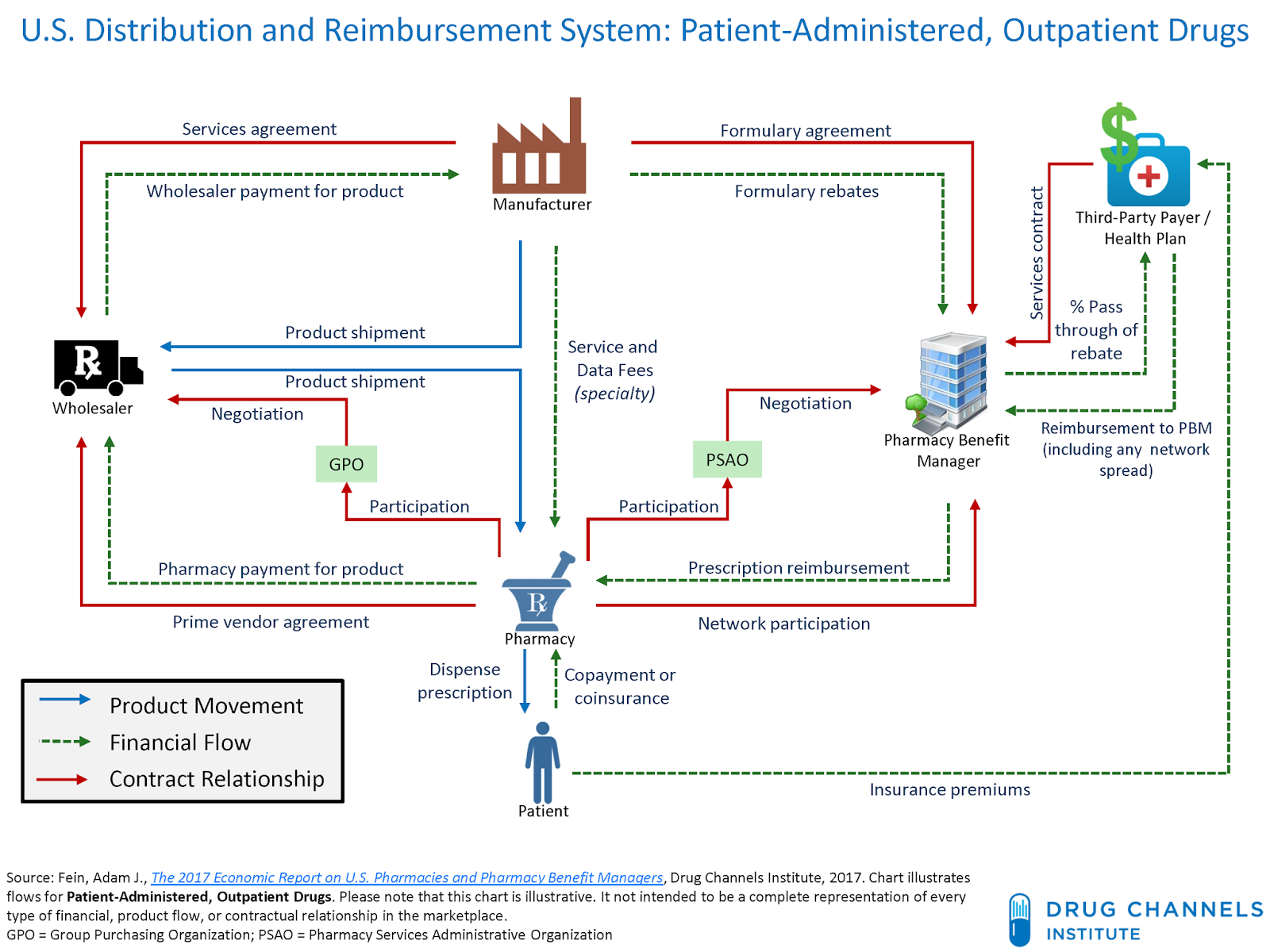
Healthcare as a Supply Chain
satya - 1/10/2022, 8:45:49 AM
Patient, Pharmacy, PBM, and Payer interaction
satya - 1/10/2022, 3:26:59 PM
Integration aspects of Payers and PBMs
1. Eligibility
2. Plans and benefits
3. Other insurances carried by members(COBs)
4. Accumulator and deductible exchanges
5. Formularies exchange
6. Rebates
7. Medical claims (likely for step therapies and other drug interactions)
8. Single sign on
9. Network data to Payer for such things as Online Provider Directories
satya - 1/10/2022, 3:29:10 PM
Notes on item 4 in the diagram above
1. The member cost share due to deductibles spent is exchanged off line, althought as soon as such a spend event occurs.
2. This means at the POS PBM directly answers the member responsibility
3. Similarly eligibility, and prior auths are also stored at PBM allowing PBM to answer the POS call from a pharmacy,
satya - 8/17/2024, 12:28:38 PM
From CAP: Center for American Progress policy institute, PBMS
From CAP: Center for American Progress policy institute, PBMS
satya - 8/17/2024, 12:30:46 PM
About CAP Briefly
- CAP - Non partisan policy institute
- Established in 2003
- Improve the lives of Americans through bold policy proposals, advocacy, and research.
- The organization addresses a wide range of issues, including economic policy, healthcare, climate change, and racial equity, with the goal of shaping national policy and fostering a more equitable society.
satya - 8/17/2024, 12:32:48 PM
At the link
- 5 Things To Know About Pharmacy Benefit Managers
- Key terms
- Available Transparency in their practices
- Price movements due to consolidation
- Money flows
- Reforms
- Broader health policy resources
satya - 8/17/2024, 12:38:57 PM
Key PBMs by market share
Key PBMs by market share
satya - 8/17/2024, 12:39:18 PM
List
- CVS Caremark
- Express Scripts (Cigna)
- Optum Rx (United Health)
- Prime (Bluecross Health plans)
- MedImpact (Independent)
satya - 8/17/2024, 12:46:52 PM
you will find
- 2017
- By Neeraj Sood, PhD, Tiffany Shih, Karen Van Nuys, PhD and Dana Goldman, PhD
- Money flow
- Profit distribution, cost
satya - 8/17/2024, 1:15:44 PM
2024 Recent prescription drug debate
- The recent agreement between Medicare and pharmaceutical manufacturers involves negotiating lower prices for ten high-cost prescription drugs as part of the Inflation Reduction Act.
- This negotiation is aimed at reducing out-of-pocket costs for Medicare beneficiaries and saving billions for the Medicare program.
- The new prices, which will be implemented in 2026, will significantly reduce the cost of these drugs, with discounts ranging from 38% to 79% off the current list prices.
satya - 8/17/2024, 1:16:17 PM
Here are the drugs
- Eliquis: For blood clot prevention, costs $521 per month, typically taken long-term for chronic conditions like atrial fibrillation.
- Jardiance: For diabetes and heart failure, costs $573 per month, usually taken long-term for chronic management.
- Xarelto: For blood clot prevention, costs $517 per month, generally taken long-term for conditions like deep vein thrombosis.
- Januvia: For diabetes, costs $527 per month, typically taken long-term as part of diabetes care.
- Farxiga: For diabetes and heart failure, costs $556 per month, generally taken long-term.
- Entresto: For heart failure, costs $628 per month, usually taken long-term.
- Enbrel: For rheumatoid arthritis and psoriasis, costs $7,106 per month, typically taken long-term.
- Imbruvica: For blood cancers, costs $14,934 per month, often taken long-term.
- Stelara: For psoriasis and Crohn?s disease, costs $13,836 per month, generally taken long-term.
- NovoLog: For diabetes, costs $495 per month, typically taken long-term.